How we can support you
In today’s healthcare market, creating efficiencies is a daily routine. More non-clinical work is being handled by physician practices to process third-party administrative work, leaving less time to treat patients. Hiring the right number of staff and/or buying new technologies to handle the increased workload can have budget consequences and put pressure on all areas of the practice. Losing a patient to another group practice is never a good thing and, in some cases, unavoidable. The cost of providing excellent clinical care today has become a challenge and will continue to be for the unforeseeable future.
A growing trend in the efficiency market is Healthcare Business Process Outsourcing. Healthcare BPO providers have specialized knowledge and expertise in streamlining processes and implementing best practices, helping group practices operate more efficiently and effectively. By outsourcing non-core functions such as appointment setting, insurance verification and authorization, medical billing, coding, and claims processing, healthcare providers can focus on their core competencies such as patient care and medical treatment.
Healthcare BPO providers typically operate in countries with lower labor costs, enabling them to offer their services at a lower cost than in-house operations. They can help group practices reduce their risk of non-compliance with regulations, billing errors, and data breaches by implementing robust compliance and security protocols.
As the fastest growing Healthcare BPO, SkyCom Healthcare can help your practice overcome these growing pains and help you rise above the competition. Think of us as your extended business office provider for all your front and back-office needs, or maybe just the most challenging part of your practice. We can help support you in multiple ways and get you back to practicing medicine and keeping your patients as healthy as possible.
Your service partner
Consultative approach
Every practice has unique needs. As such, we offer a consultative approach to all projects we take on. Our solutions are customized to ensure your patients receive the best CX journey from first point of contact to receiving their first billing statement.
Omni channel solutions
Your patients use different platforms and have different communication preferences. We offer a fully equipped contact center offering omnichannel solutions to serve the communication needs of all your clients, 365 days per year 24/7.
Increased returns
With service centers across, we can offer you the best bilingual support for a fraction of your local cost. This enables you to deploy more agents, improve your customer service and ultimately increase revenue.
SkyCom Healthcare core capabilities

SkyCom Healthcare core capabilities

SkyCom Healthcare core capabilities
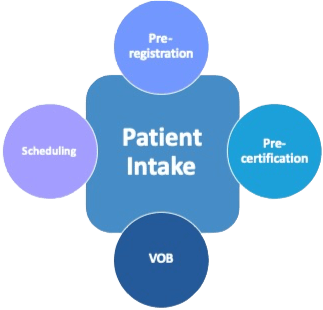
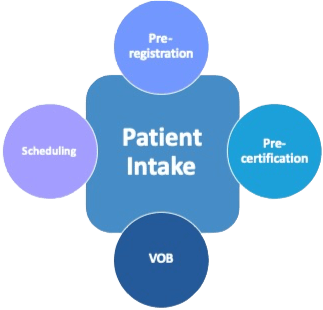
Patient
Intake
Scheduling
VOB
Pre-registration
Pre-certification
EOB/ERA Reviews
Collections
837 Billing
Denial management
Document management
Scheduling
Our scheduling teams are responsible for maintaining a <3% call abandonment rate across all US time zones. We also operate outreach programs to bring lost patients back to the practice, in addition to making a post visit follow-up touchpoint.
Pre-registration
New or existing patients should not have to fill out registration paperwork in your lobby. Nor should your staff need to collect their co-payment or deductible upon their arrival. Let us register them in your CRM and collect their out of pocket expense before their appointment as it should be.
Pre-certification
Although an authorization number is not a guarantee of payment, it definitely is a common denial without one. Let us ensure that every visit is authorized so that more of your claims are paid on time.
Verification of Benefits
It is common for patients to continue using insurance cards for policies they no longer have. Secondly, patients are purchasing plans with less benefits to take advantage of lower premiums without knowing the details of what they purchased. Our VOB team can easily verify benefit levels and deductible/co-insurance amounts and reschedule patients who may not have adequate medical coverage.
837 Billing
In a typical physician office, the billing function is combined with collections. We believe that billers should be dedicated entirely on billing as there are multiple billing workflows that often get missed (i.e. acceptance/rejection reports, 277 reports, rebilling requests). Our dedicated billing teams are trained to complete all billing functions within multiple billing and clearinghouse platforms.
Document management
Physician offices typically receive dozens of document requests daily. With each request having a specific turnaround period, many requests are not fulfilled timely and can jeopardize claim reimbursement. Let our document fulfilment team get your request processed and submitted within 48 hours of notification.
EOB/ERA Reviews
Incorrect payment posting and/or incorrect claim adjudication can be a result many different things. Our EOB/ERA teams are trained to spot inconsistences and provide valuable feedback can help capture lost revenue.
Denial management
Any claim that is not paid within 30-45 days of submission is a denial. Our collection-denial management teams have extensive experience in filing appeals with all the appropriate documentation. In addition, most payer web portals do not provide updated claim information on appealed claims and require an actual phone call for claim status. Let us chase down your denials and help recover cash that over time may not be recoverable.
Any claim that is not paid within 30-45 days of submission is a denial. Our collection-denial management teams have extensive experience in filing appeals with all the appropriate documentation. In addition, most payer web portals do not provide updated claim information on appealed claims and require an actual phone call for claim status. Let us chase down your denials and help recover cash that over time may not be recoverable.
Additional capabilities
Telehealth Adoption Programs
In the new age of Covid-19, first visit adoption programs, including pre-calls with members/patients, and where applicable with Doctors, is essential. Let us walk them through the technology and “what to expect” on their first healthcare visit. Our research shows that these pre-calls were able to establish comfort, rapport and ease of use that saw >60% lift in repeat user adoption over prior processes.
Telehealth Tech Support
While many Provider groups have their own IT, they are typically overburdened and unable to provide the immediate tech support response required for telehealth needs of everyone. We can provide the skilled resources to respond to issues (i.e. “I can see, but not hear the patient”). Where the issue is internal to the provider firewall, we can initiate the trouble ticket and track it for the clinician and subsequently reschedule the visit.
Clinical Device Tech Support
We provide tier 0 (FAQs, self-service) up to more complex tier 2 multichannel tech support for clinical devices to both consumers and in clinical or B2B environments.
RDM/RPM & Coaching
Let us support your chronic care patients currently on a clinical care plan through Remote Device Monitoring and Coaching. Our team can help patients get set up on monitoring devices, then coach them to a weekly plan for better health outcomes with the ability to escalate back into clinicians when appropriate. Based on new financial incentives in the latest Medicare provisions, lifecycle patient management programs create a win-win situation for everyone.
Medicare, Medicaid & PBM
We can serve key member/patient queries for Medicare, Medicaid and Pharmacy Benefit Management requirements all within a compliant and secure environment.
After Hours Contact Center
Our IT consulting team can help design a customized plan to support members and patients after regular services hours, with options for appointment setting, rescheduling, escalations, credentialing and more. Elevating care and satisfaction well beyond the old and ineffective answering service model is what your practice deserves.
Full Revenue Cycle Management
Our AR consulting team can quickly develop an AR reduction plan that utilizes time, payer conditions, and client needs to increase cash collections and reduce AR days. What’s unique about our service is that we can create both the plan and execute an operations team to stand up a pilot in less than 30 days.
Case study
Effecting a business model change through improved collections
HIPAA Compliance
SkyCom Healthcare understands the importance of keeping patient information private. We strictly adhere to the guidelines as set forth by the Health Insurance Portability and Accountability Act to ensure that a patient’s Protected Health Information is collected, stored and transmitted with the utmost of security. As a HIPAA compliant call center we can help accelerate the cycle of communication, optimize workflow, and increase patient service levels. Our clients rely on our expertise to make certain they exceed regulations, in turn lowering the risks for security breaches and patient disappointment.
At SkyCom Healthcare only a select of group of agents are permitted have access to patient information and engage callers over our secure communications network. Regular trainings are also provided to our agents regarding information security with an emphasis on Personal Health Information. Regular Trainings and staff education ensure compliance of all related obligations under HIPAA.
Our comprehensive internal policies paired with our technology, security and privacy policies all comply with HIPAA standards. All this, paired with discipline is what allows us to maintain and manage a compliant operation that is heads and shoulders above the competition.